About Conference
With absolute enthusiasm and the Will to influence, we extend a warm welcome to all attendees of 9th International Conference on Tropical Medicine and Infectious Diseases scheduled on August 26-27, 2020 in the beautiful city of Singapore.
This year we came up with the refreshing theme on “Tackling Challenges and Future aspects on Tropical Medicine and Infectious Diseases”.
Tropical Medicine 2020 is all set to bring together the eminent scholars from the Infectious department and Tropical Medicine community presenting the unsurpassed opportunities to present and explore the future Front line technologies on Tropical medicine and Infectious Diseases
Witness the gathering the world-leading and renowned academicians, business delegates, principal investigators, nurses, homeopathists, researchers, students to witness the futuristic ideologies put forth by the experts.
This integrative 2-day event deliberates the new strategies, convictions that will impact the process of your professional development. Join us with and share your research and business tactics which will direct to the optimistic approach to the advancements on Tropical Medicine and Infectious Diseases
Connect with us to Socialize, Interact, Network and Collaborate at Tropical Medicine 2020.
We look forward to hosting you in Singapore!
Regards
|
Conference series LLC Ltd with the astounding and awesome feedback from the Tropical Medicine 2019, we would like to announce the commencement of our next series 9th International Conference on Tropical Medicine and Infectious Diseases is going to organize in the Lion City of Singapore on August 26-27, 2020.
Tropical Medicine 2020 is a technical Conference which includes keynote presentations, general oral presentations, poster sessions, workshops, exhibitions, panel discussions from specialists of Epidemiologists, Pathologists, Infectious disease departments, gastroenterologists, neurologists, pediatricians and other partnered arenas of Tropical Science.
The main perspective of this conference is to provide a great platform, Academicians, Researchers, Scientists, Industrial Professionals and students to unleash their research work and create a forum for effective sharing of ideas to face the future global challenges from the perspective of rising trends in engineering and technology. Tropical Medicine 2020 highlights the ever-increasing and basic need to energize creative engineering solutions with potential for worldwide reach. This would be a wonderful opportunity for networking and will cultivate everlasting friendships among fellow partners.
- Opportunity to sharpen your saw by learning new skills in International environment
- Can learn new information and tactics from other presentations at Tropical Medicine conference
- Can converse with Tropical Medicine scientists from various universities and even countries you may have only heard or read about
- It helps to improve your research work by getting feedback from the experts and influencers in the field of Tropical Medicine.
- Opportunity to visit Singapore where the conference is being held and learn about its people, culture, and attractions
- Great opportunity to connect with attendees from different views and perspectives, make new relationships, and strengthen existing ones
- Accelerate academic reputation
- Direct introductions, meeting with present and potential researchers, making a sprinkle with new advancements and name acknowledgment are the signs of this two days occasion.
Conference Highlights
- Nosocomial Infections & Control
- Infectious Diseases
- Pediatric Infectious Diseases
- Global Markets on Infectious Diseases
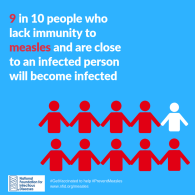
- Immunology of Infections
- Neuro Infectious Diseases
- Veterinary Infectious Diseases
- Bacterial Infectious Diseases
- Fungal Infectious Diseases
- Blood infectious Diseases
- Advancements in Vaccines and Therapeutics
- Molecular Diagnosis and Treatment of Infectious Diseases
- Antimicrobials/Antibiotics/Antibacterial
- Infectious Diseases Epidemiology
- Viral Infectious Diseases
- Ebola and Zika Viral Infections
- Dental and Oral Infectious Diseases
- Tropical Medicine and Immunization Vaccination
- Neglected Tropical Diseases
- Most Common NTDs Causes and Treatments
- Infection Control And Public Health Awareness
- HIV/AIDS and Sexually Transmitted Infections
Special Issues
· All accepted abstracts will be published in respective Supporting International Journals.
· Abstracts will be provided with Digital Object Identifier by Cross Ref.
See more at:- https://tropicalmedicine.infectiousconferences.com/